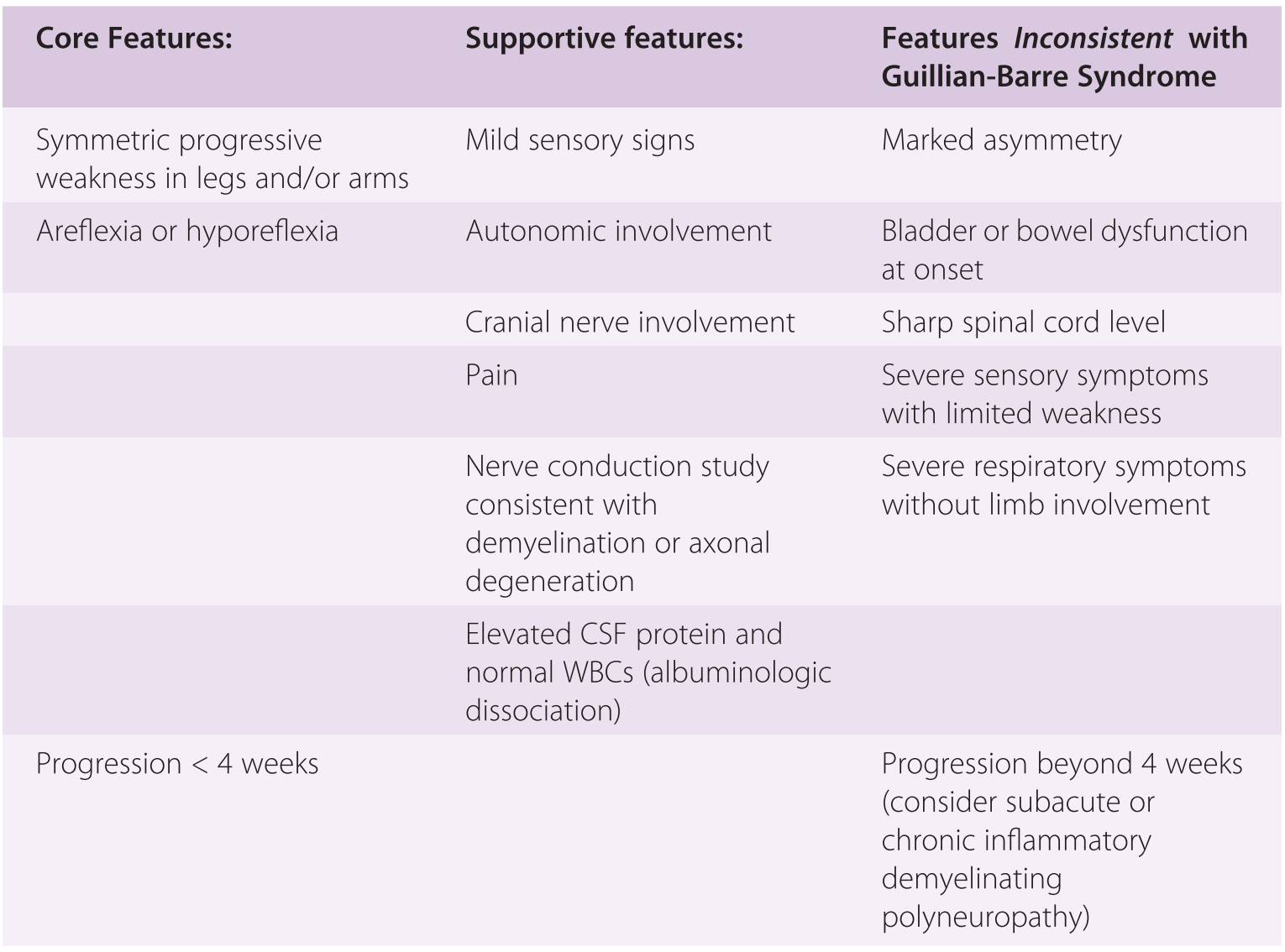
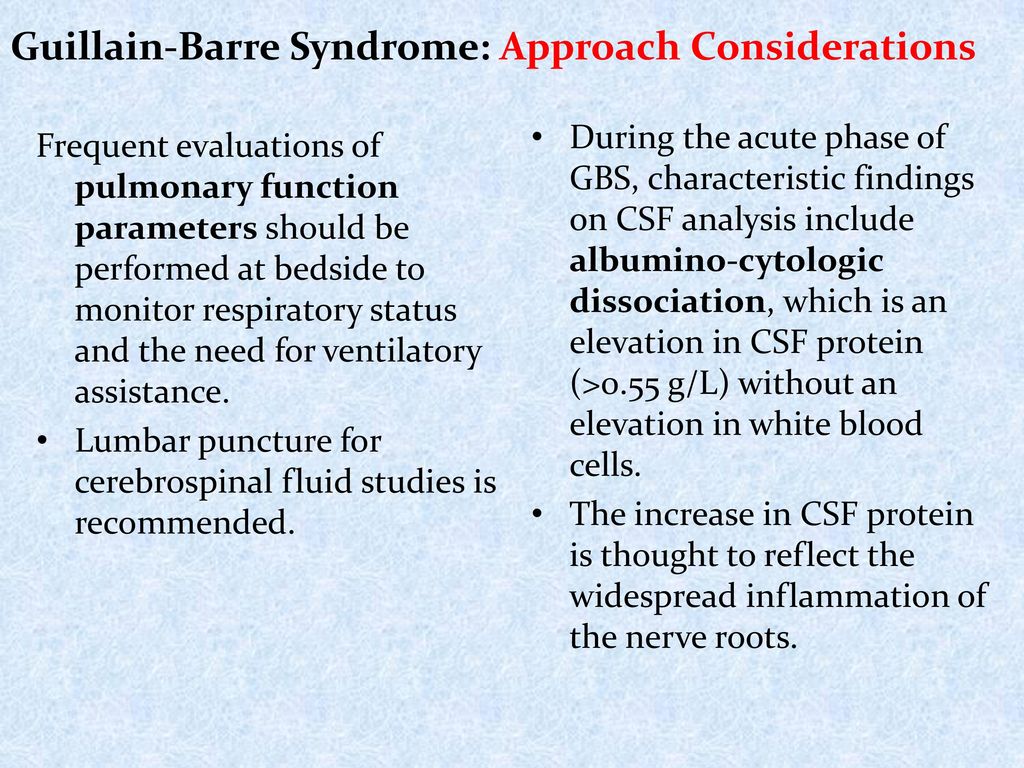
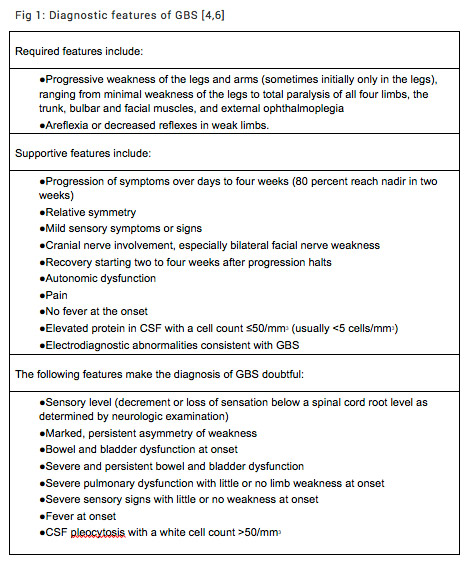
Eventually an MRI demonstrated abnormal spinal nerve roots, and a lumbar puncture confirmed an elevated CSF protein level in the absence of inflammatory cells Persistent, painful dysfunction without complete paralysis has a broad differential diagnosis that includes several conditions that are far more common than GuillainBarré syndrome CSF protein elevation in GBS is thought to be due to bloodnerve barrier disturbance and damage to the peripheral nervous system at the level of the nerve roots In addition, the presence of high levels of neurofilament proteins in CSF has been associated with poor clinical and electrodiagnostic outcomes 14, 15A level 2 diagnosis is supported by either a CSF whitecell count of less than 50 cells per cubic millimeter (with or without an elevated protein level) or by results of nerveconduction studies
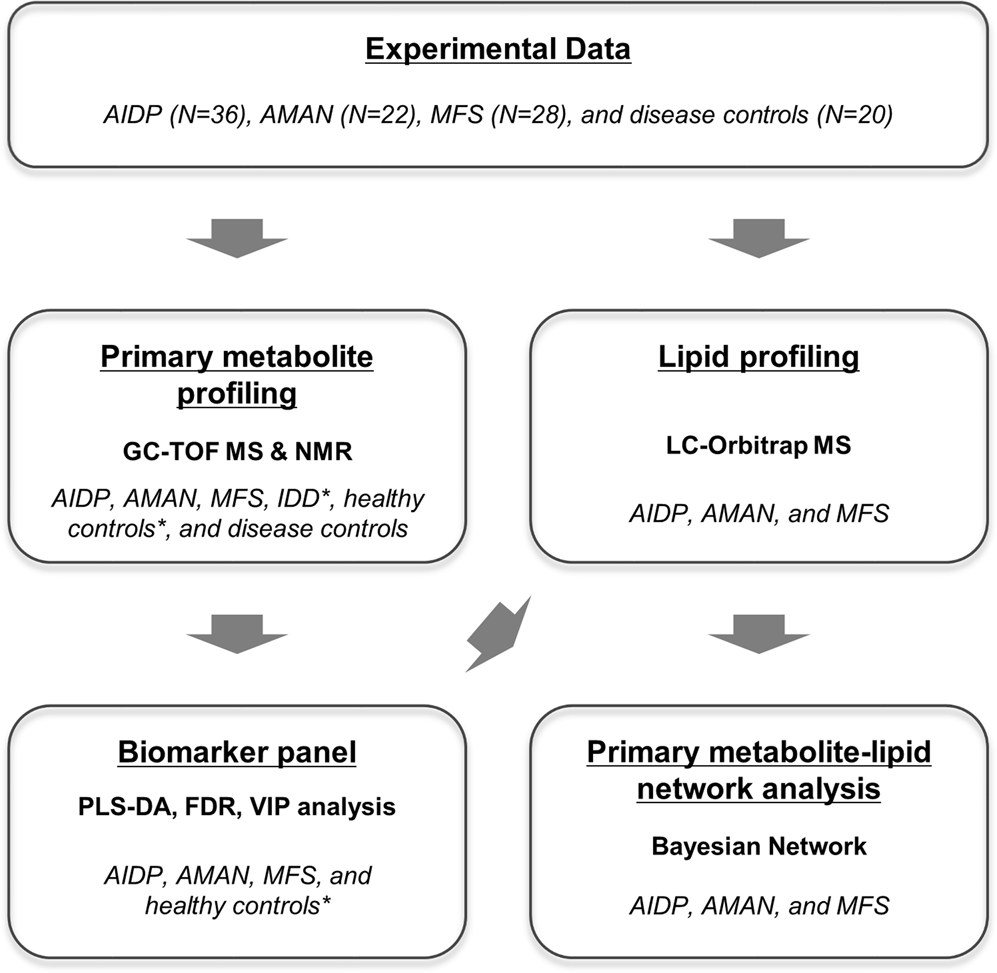
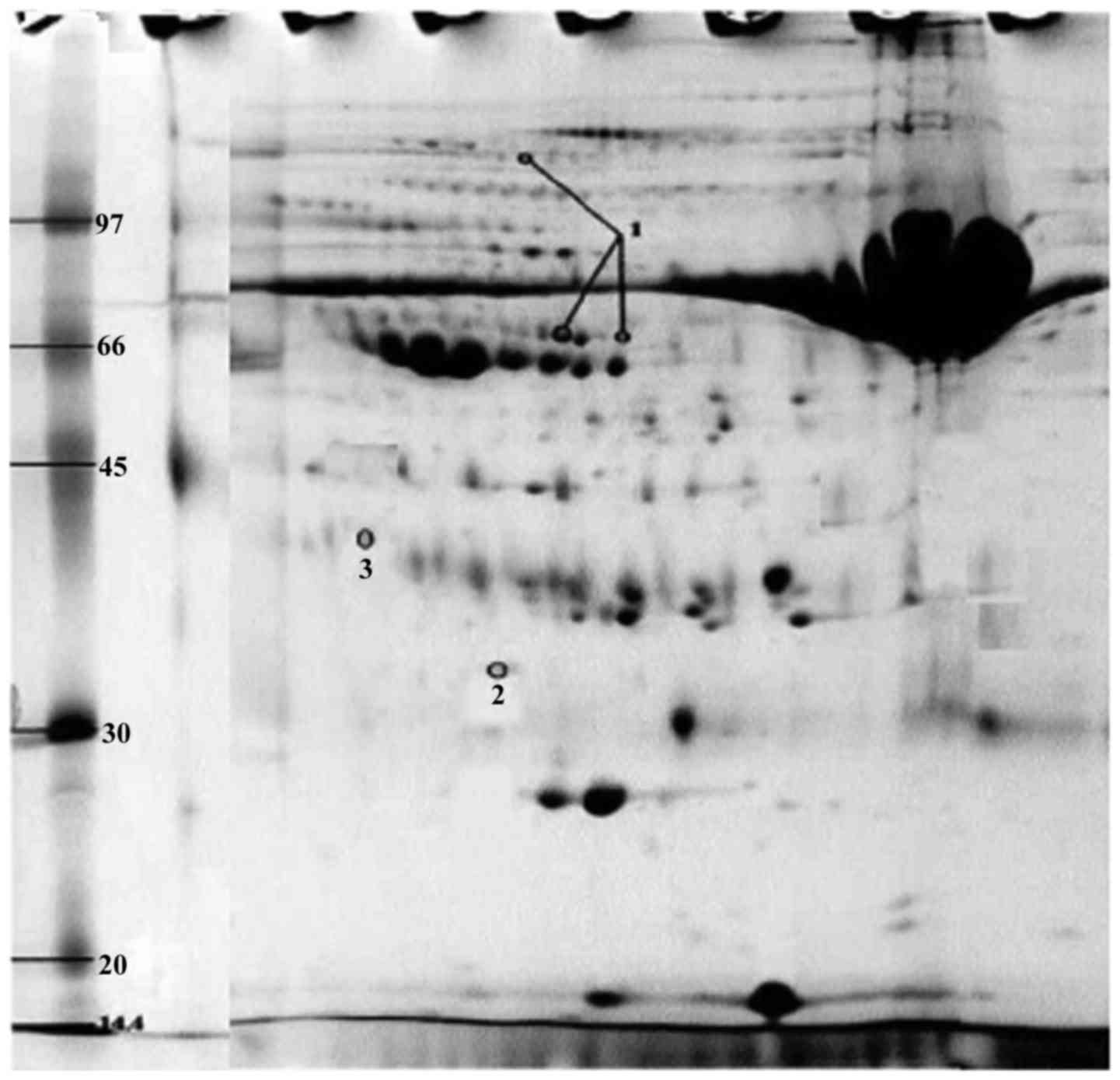
Integrative Metabolomics Reveals Unique Metabolic Traits In Guillain Barre Syndrome And Its Variants Scientific Reports
Why is csf protein elevated in gbs
Why is csf protein elevated in gbs- GuillainBarré syndrome (GBS) is a rare neurological disorder in which the body's immune system mistakenly attacks part of its peripheral nervous system—the network of nerves located outside of the brain and spinal cord GBS can range from a very mild case with brief weakness to nearly devastating paralysis, leaving the person unable toHigh protein level in cerebrospinal fluid (CSF) (the fluid that surrounds the spinal cord and brain) To diagnose GBS, you may have the following tests Spinal tap (lumbar puncture) A special needle is placed into the lower back, into the spinal canal This is the area around the spinal cord



Integrative Metabolomics Reveals Unique Metabolic Traits In Guillain Barre Syndrome And Its Variants Scientific Reports
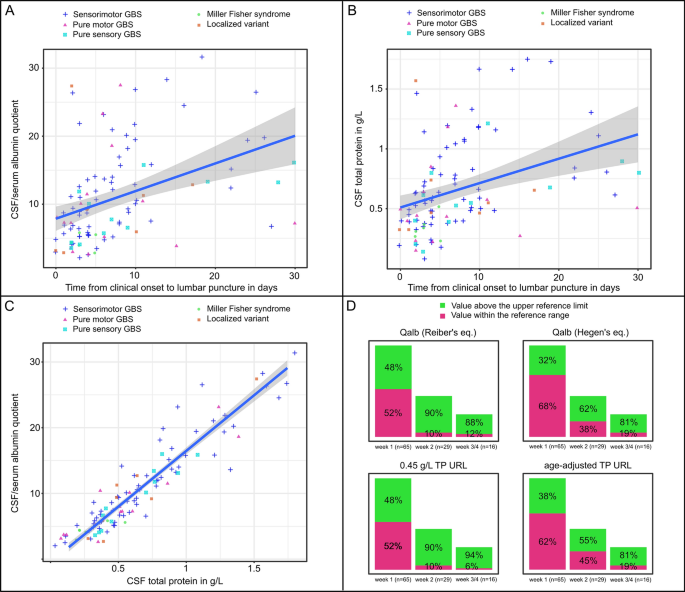
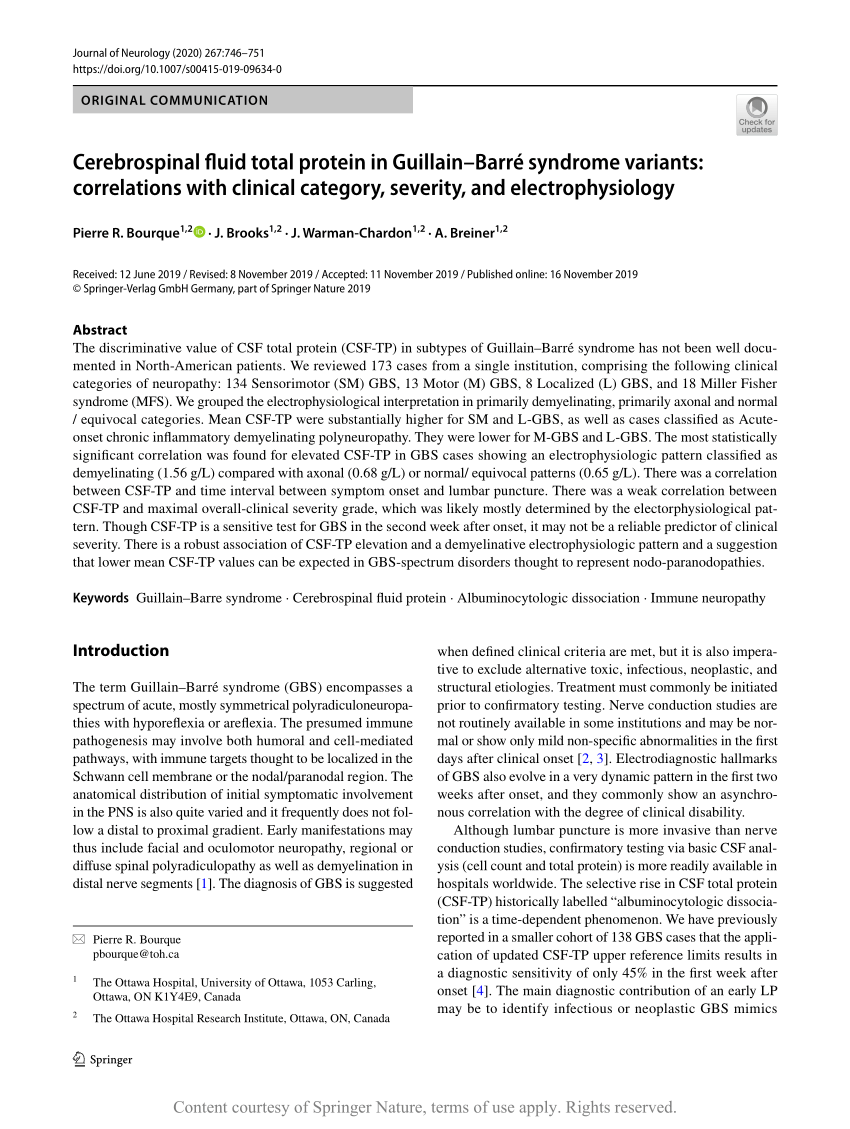
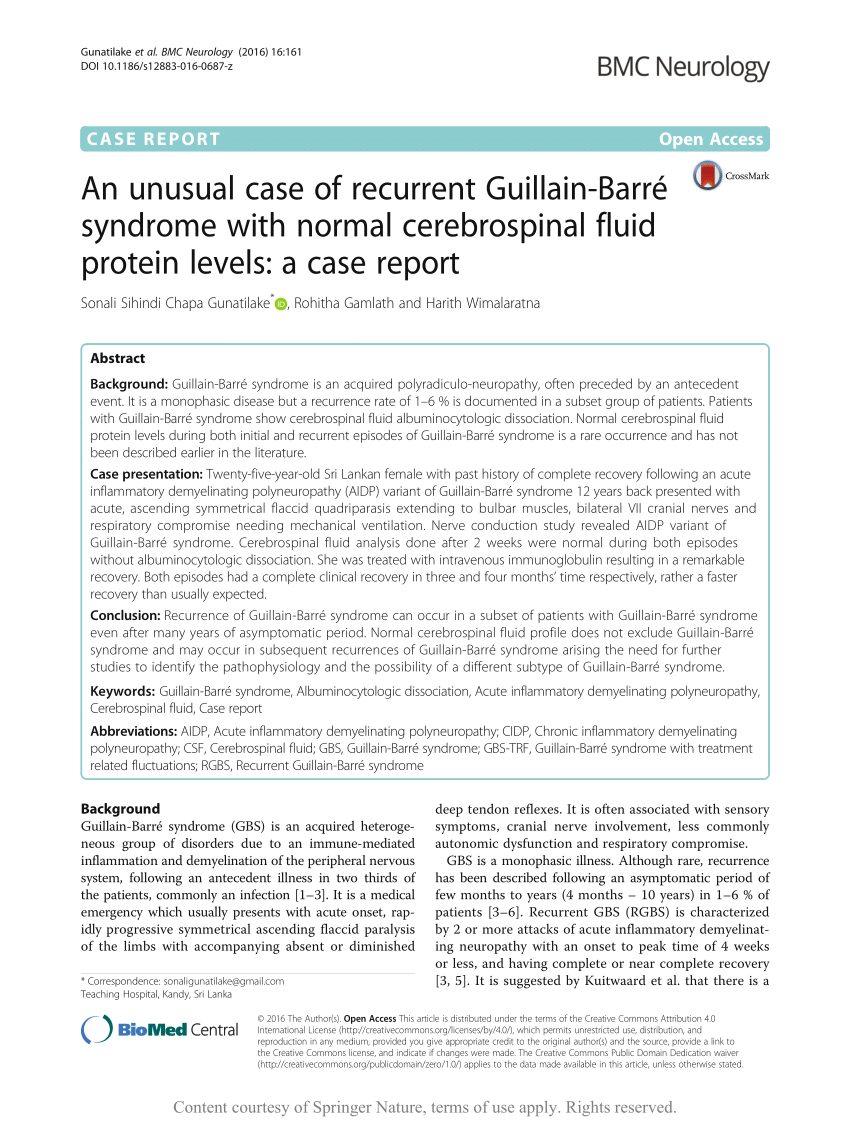
Objectives The cerebrospinal fluid (CSF) protein level is known to be elevated in patients with Guillain–Barré syndrome (GBS) This report correlates the degree of CSF protein elevation with the number of electrophysiologic abnormalities on nerve conduction study (NCS) Methods We reviewed 38 patients admitted to our institution with a diagnosis of GBS and had both a measured CSF proteinCSF results for a patient with GB would reveal increased protein levels and a normal cell count For each option, select the correct assessment or test result for a patient who has been diagnosed with GuillainBarré syndrome (GB) and is exhibiting clinical symptoms of paralysisExtremely high protein levels (10 g/L 1000 mg/dL) are associated with development of high intracranial pressure and papilloedema Around 10% of patients will not have a protein elevation, including patients with the MillerFisher variant 15 Ropper A, Wijdicks E,
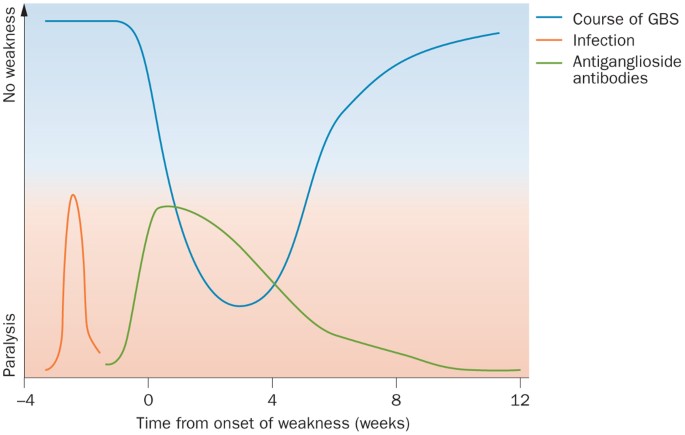
Cerebrospinal fluid (CSF) total protein level and plasma neutrophil/lymphocyte ratio (NLR) are related with autoimmune response We aimed to reach a prognostic indicator for GBS by using electrophysiological findings, protein level of CSF, and plasma NLR based on Medical Research Council (MRC) sum score dataGuillain‐Barré Syndrome (GBS) is a rare autoimmune inflammatory polyneuropathy with a high risk of respiratory failure and unclear pathogenesis were down‐regulated in the CSF of the GBS patients The CSF haptoglobin level, quantified by enzyme‐linked immunosorbent assay, was significantly This study indicated that protein GBS Guillain Barre Syndrome causes albuminocytologic dissociation, which means an increase in the concentration of the cerebrospinal proteins without an associated increase in the white blood cells An increase in protein concentration is directly proportional to an increase in inflammation of the nerve cells
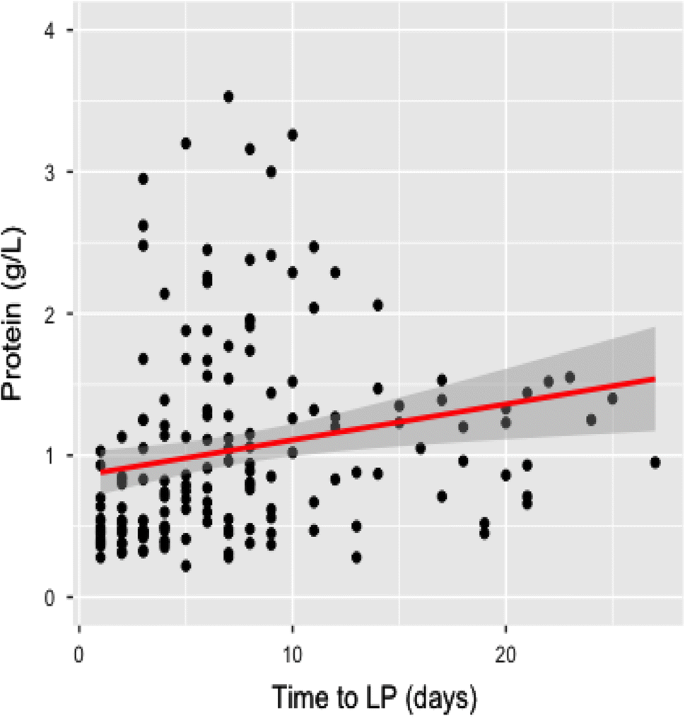
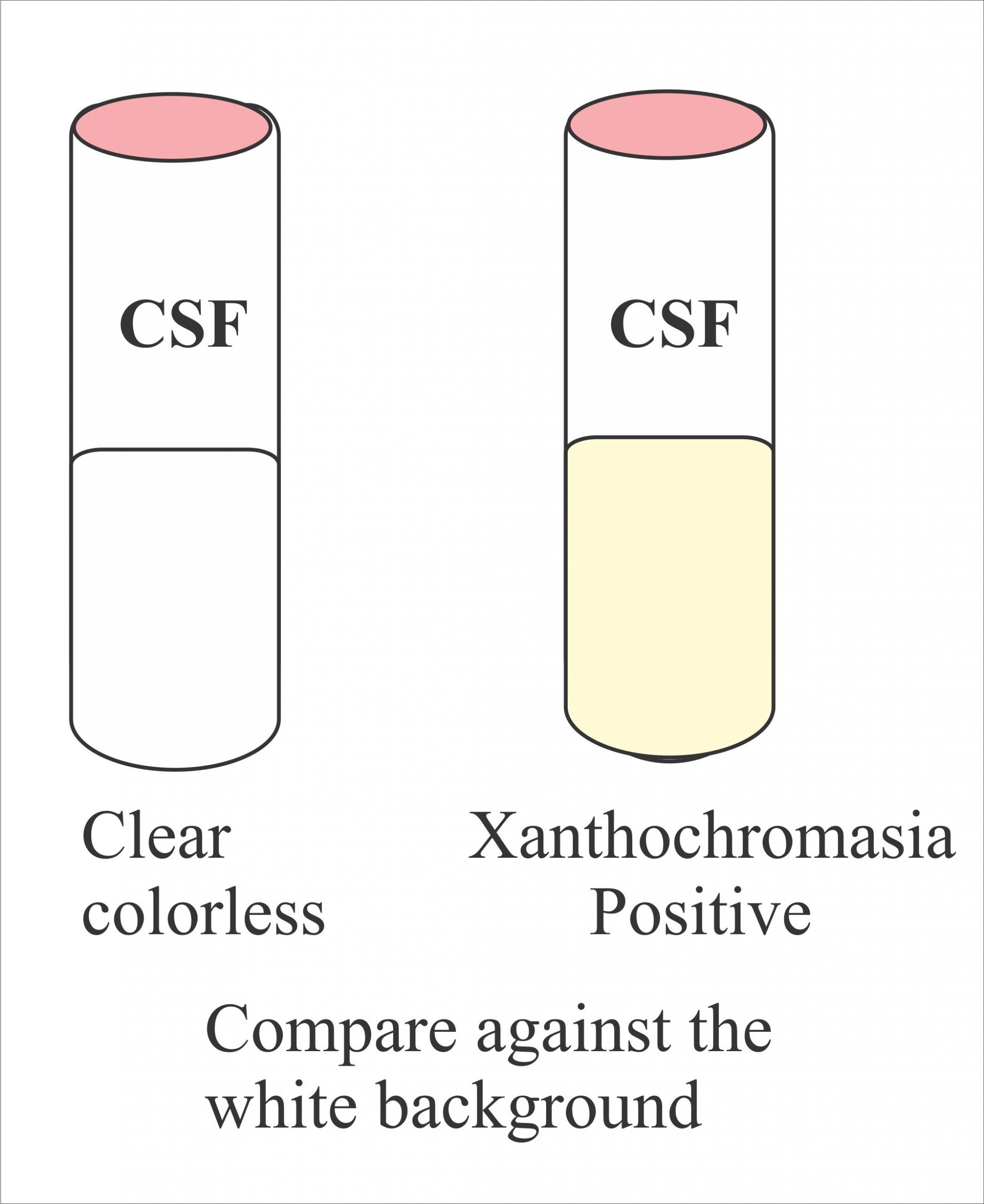
Local clinical care facilities and treatment options may also influence the clinical course and outcome of GuillainBarré syndrome CSF examination may be useful in cases of clinical uncertainty Despite this, the CSF is unremarkable in 50% of people with Guillain–Barré syndrome in the first few days of symptoms, and 80% after the first week;CSF protein is usually normal within the first 23 days but then begins to rise very quickly, reaching a peak at 46 weeks and then persisting at a variably elevated level for many weeks 15 CSF protein level varies from 45 to 300 mg/dL, but levels as high as 1000 mg/dL can be seen 144




Pdf Are Cerebrospinal Fluid Protein Levels And Plasma Neutrophil Lymphocyte Ratio Associated With Prognosis Of Guillain Barre Syndrome Semantic Scholar




Age Matters Neurology Neuroimmunology Neuroinflammation
Guillain‐Barre syndrome (GBS) is one such complication that has been reported from different parts of the world We are a tertiary‐care University Hospital, serving additionally as an apex (Level 3 unit) COVID‐19 referral facility,in the Northern part of IndiaTherefore, normal results do not exclude the condition Repeating the lumbar puncture during the disease course is not recommended The protein levels may rise after treatment has been administered Spinal tap was performed on day two of admission, and cerebrospinal fluid (CSF) analysis showed an elevated protein level ( mg/dl) with no cells in accordance with albuminocytologic dissociation Antigangliosides antibodies were not checked



Csf Findings In Guillain Barre Syndrome Demyelinating And Axonal Acute Inflammatory Polyneuropathies Springerlink




Causes Of Albuminocytological Dissociation And The Impact Of Age Adjusted Cerebrospinal Fluid Protein Reference Intervals A Retrospective Chart Review Of 2627 Samples Collected At Tertiary Care Centre Bmj Open
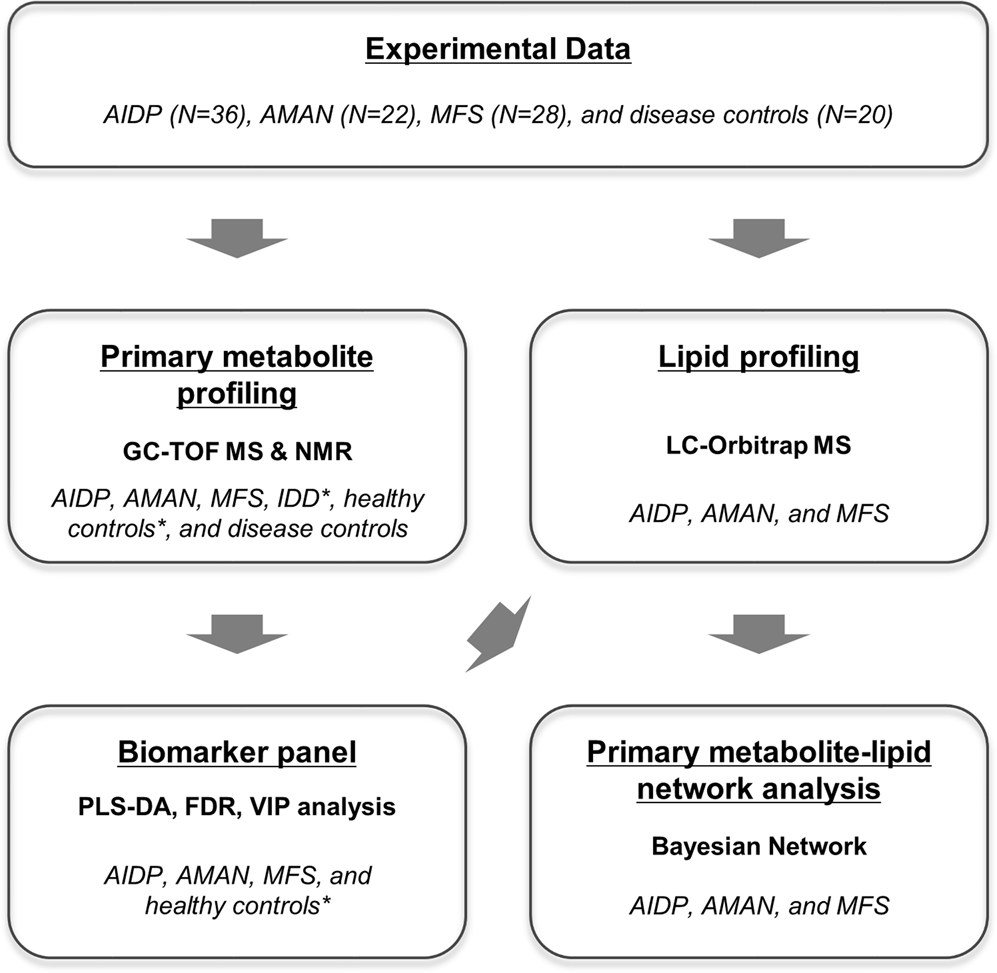
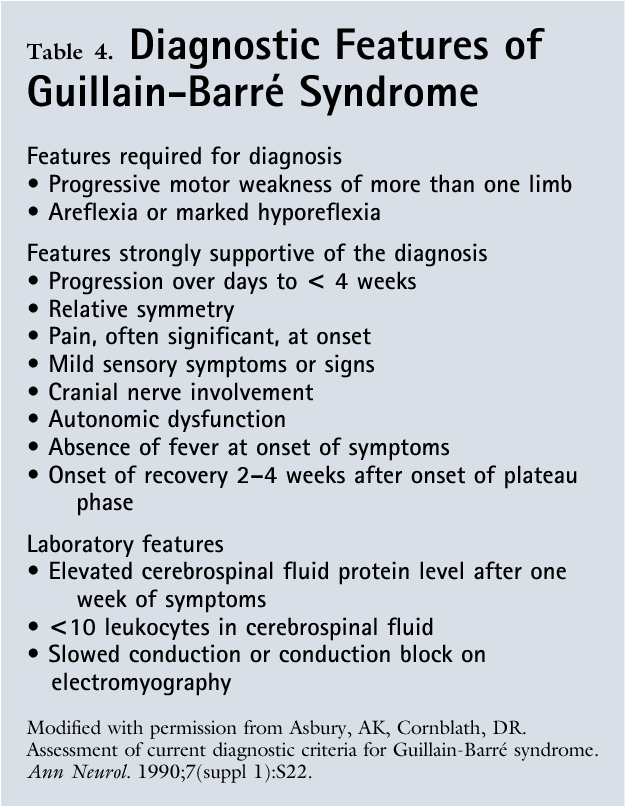
GuillainBarré syndrome is the most common and most severe acute paralytic neuropathy, with about 100 000 people developing the disorder every year worldwide Under the umbrella term of GuillainBarré syndrome are several recognisable variants with distinct clinical and pathological features The severe, generalised manifestation of GuillainBarré syndrome with respiratoryIn patients with serial nerve conduction studies, the study around 2 weeks after onset of weakness was chosen for the Brighton classification CSF count and protein concentration were determined by routine diagnostic methods The normal value for CSF protein concentration was 018–058 g/lGuillainBarre syndrome (GBS), or acute idiopathic polyneuritis, is characterized by ascending symmetric paralysis Respiratory involvement may be absent, or it may be severe enough to necessitate mechanical ventilation Seventy percent of cases are preceded by



Identification Of Csf Biomarkers By Proteomicsin Guillain Barre Syndrome



Http Www Bioline Org Br Pdf Ni
Guillain Barré syndrome (GBS) is a postinfectious acute autoimmune polyradiculopathy Cerebrospinal fluid (CSF) total protein level and plasma neutrophil/lymphocyte ratio (NLR) are related with autoimmune response Rajabally YA, Uncini A Outcome and its predictors in GuillainBarre syndrome Journal of neurology, neurosurgery, and psychiatry 12; The classic immunologic alteration of the cerebrospinal fluid (CSF) in Guillain–Barré syndrome (GBS), albuminocytologic dissociation, has been known since the original paper by Guillain, Barré



Guillain Barre Syndrome And Myasthenia Gravis Chapter 43 Gupta And Gelb S Essentials Of Neuroanesthesia And Neurointensive Care




Guillain Barre Syndrome Mimics Tham 18 Brain And Behavior Wiley Online Library
12 rows CSF total protein lim = 0124 × age − 708 × 10 −4 × age 2 3 × 10 −6 × age 3 −Factors associated with prognosis of GuillainBarre syndrome Naglaa Mohamed ElKhayat, Maha Ali Nada*, Heba Hamed ElSayed, Lower albumin level, higher CSF protein level and of course axonal affection in nerve conduction study However, the degree of cytoalbuminous dissociation didn't show a significant difference between the The CSF is acellular in all but 10% of patients, who may have 11 to 50 cells/mm3 About 1 week after the onset of symptoms, the protein levels rise, reaching a peak in 3 to 4 weeks Pleocytosis may signify Lyme disease, sarcoid, neoplasia, GuillainBarré syndrome associated with HIV, EpsteinBarr virus, or other diseases




Clinical Features And Prognosis With Guillain Barre Syndrome




Guillain Barre Syndrome Rcemlearning
Prognosis in GuillainBarré syndrome patients We defined an elevated CSF protein level as higher than 045 g/L 15 21 Clinical variants were defined as sensorimotor, pure motor, pure sensory, MFS, ataxic and pharyngealcervical brachial variant 22 NCS results were classified as acute inflammaGuillain Barré syndrome (GBS) is a postinfectious acute autoimmune polyradiculopathy Cerebrospinal fluid (CSF) total protein level and plasma neutrophil/lymphocyte ratio (NLR) are related with autoimmune response We aimed to reach a prognostic indicator for GBS by using electrophysiological findi Guillain Barré syndrome (GBS) is a postinfectious acuteThis pattern distinguishes Guillain–Barré syndrome from other conditions (such as lymphoma and poliomyelitis) in which both the protein and the cell count are elevated Elevated CSF protein levels are found in approximately 50% of patients in the first 3 days after onset of weakness, which increases to 80% after the first week




An Unusual Case Of Recurrent Guillain Barre Syndrome With Normal Cerebrospinal Fluid Protein Levels A Case Report Semantic Scholar
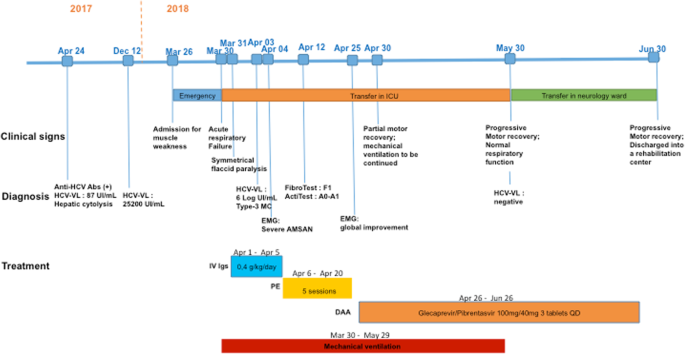



Severe Guillain Barre Syndrome Associated With Chronic Active Hepatitis C And Mixed Cryoglobulinemia A Case Report Bmc Infectious Diseases Full Text
GuillainBarré Syndrome ICM Case Summaries Leave a comment A sixty year old man was admitted to the ITU with respiratory failure He initially presented with a week long history of limb weakness that started in his legs CSF sampling showed elevated protein levels and a diagnosis of GuillainBarréNormal cerebrospinal fluid protein levels during both initial and recurrent episodes of GuillainBarré syndrome is a rare occurrence and has not been described earlier in the literature During the acute phase of GBS, characteristic findings on CSF analysis include albuminocytologic dissociation, which is an elevation in CSF protein (>055 g/L) without an elevation in white blood



Frontiers Trauma Related Guillain Barre Syndrome Systematic Review Of An Emerging Concept Neurology




Cerebrospinal Fluid Protein In Guillain Barre Syndrome Need For Age Dependent Interpretation Hegen 21 European Journal Of Neurology Wiley Online Library
High protein level in cerebrospinal fluid (CSF) CSF is the fluid that surrounds the spinal cord and brain To diagnose GBS, you may have the following tests GuillainBarré syndrome (GBS) is a neurological disorder in which the body's immune system attacks part of the peripheral nervous systemHigh protein level in cerebrospinal fluid (csf) (the fluid that surrounds the spinal cord and brain) To diagnose gbs, you may have On auscultation and flaccid muscle tone and sensory loss in all extremitiesChisquare test was applied to a number of demyelination criteria and Ttest/ANOVA was applied on mean CSF protein level Results We found a mean CSF protein of 3741 mg/dl (±369) with one




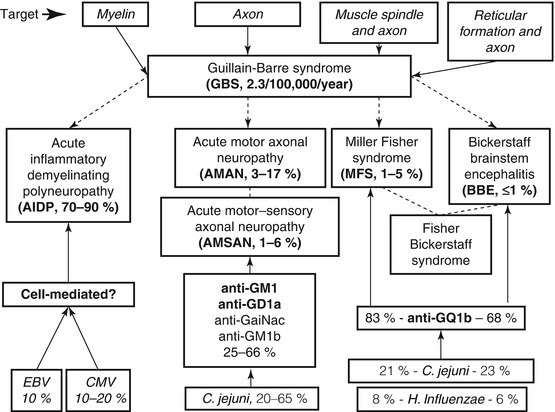
The Pathogenesis Of The Demyelinating Form Of Guillain Barre Syndrome Gbs Proteo Peptidomic And Immunological Profiling Of Physiological Fluids Molecular Cellular Proteomics



Guillain Barre Syndrome Calgary Guide
The classic finding is albuminocytologic dissociation (elevated protein, despite normal cell count) Protein is usually elevated, up to very high levels (1001,000 mg/dL) Elevated protein has a sensitivity of ~50% during the first week,Of GuillainBarre Syndrome tar responses, and illdefined sensory levels are demonstrable, and these need not exclude the B Cerebrospinal fluid features strongly supportive of the diagnosis 1 CSF protein After the first week of symptoms, CSF protein is elevated or has been shown toGuillainBarré syndrome (GBS) is an acute inflammatory polyneuropathy affecting the myelinprotein sheathing and the axons themselves to various degrees Damage to these structures causes biomarkers to be released into the adjacent body fluid compartment In case of the proximal nerve roots these bi



3




Guillain Barre Syndrome American Family Physician
A level 2 diagnosis is supported by either a CSF whitecell count of less than 50 cells per cubic millimeter (with or without an elevated protein level) or by results of nerveconduction studiesGuillainbarre syndrome (gbs) and Paresthesias of trunk or face unusual, but sensory loss over the trunk Loss of reflexes;(7)7118 PMID Raphaël JC, Chevret S, Hughes RA, et al Plasma exchange for GuillainBarré syndrome The Cochrane database of systematic reviews 12;



An Unusual Case Of Recurrent Guillain Barre Syndrome Of A Different Subtype Five Years After Initial Diagnosis Manorenj Journal Of Pharmaceutical And Biomedical Sciences




Supplemental Materials For Distal Limb Weakness Phenotype Of Guillain Barre Syndrome Journal Of The Neurological Sciences
A If CSF is not collected or results not available, nerve electrophysiology results must be consistent with the diagnosis GuillainBarré syndrome Open in new tab Table 1 Key diagnostic criteria and Brighton case definitions for GuillainBarré syndrome Level of diagnostic certainty Hydrocephalus and pseudotumour cerebri are a rare complication of GuillainBarré syndrome (GBS), occurring in about 4% of the cases The high concentration of cerebrospinal fluid (CSF) protein may lead to a decreased CSF absorption in arachnoid villi A 10yearold boy with GBS and hydrocephalus is presentedObjective GuillainBarré syndrome (GBS) is an autoimmune disease characterized by weakness in limbs or cranial nerve innervated muscles Acute inflammatory demyelinating polyradiculoneuropathy (AIDP) is the most common variant Electrophysiologic abnormalities and elevated cerebrospinal fluid (CSF) protein are frequently present in AIDP, but the relationship




Guillain Barre Syndrome Mayo Clinic Proceedings
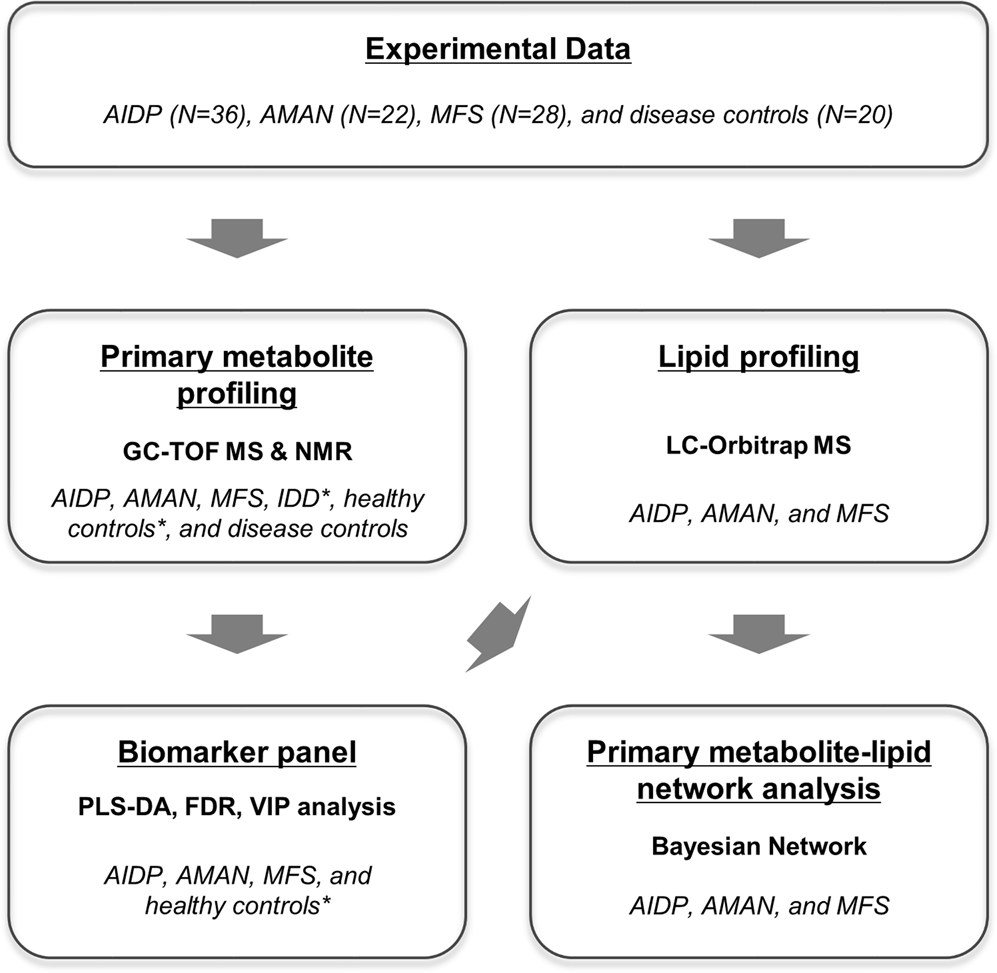



Integrative Metabolomics Reveals Unique Metabolic Traits In Guillain Barre Syndrome And Its Variants Scientific Reports
GuillainBarré syndrome (GBS) is an eponym for a heterogeneous group of immunemediated peripheral neuropathies A feature common in all GBS variants is a rapidly evolving polyradiculoneuropathyIf CSF White cell count significantly raised consider HIV/Lyme as well Differential Diagnosis Patients with a sensory level on the trunk must be considered to have a spinal cord lesion until proven otherwise GuillainBarre Syndrome patients do not usually have a sensory level Weakness with facial involvement may be caused by brainstem CSF hypocretin1 was measured in 28 GuillainBarré syndrome (GBS), 12 MillerFisher syndrome, 12 chronic inflammatory demyelinating polyneuropathy (CIDP), and 48 control subjects Seven GBS subjects had undetectably low hypocretin1 levels (




Guillain Barre Syndrome Rcemlearning




Guillain Barre Syndrome Csf Mundo Das Entrevistas




Guillain Barre Syndrome



Emdocs Net Emergency Medicine Educationguillain Barre Syndrome Third Time S The Charm Emdocs Net Emergency Medicine Education



Emdocs Net Emergency Medicine Educationguillain Barre Syndrome Third Time S The Charm Emdocs Net Emergency Medicine Education




Guillain Barre Syndrome Teesneuro Org




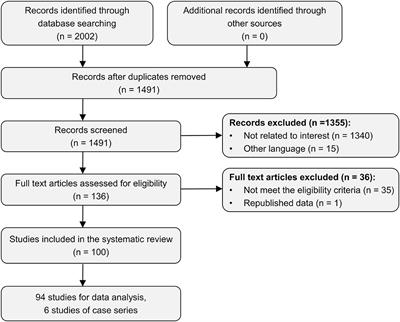
Guillain Barre Syndrome And Its Variants As A Manifestation Of Covid 19 A Systematic Review Of Case Reports And Case Series Journal Of The Neurological Sciences




Guillain Barre Syndrome Case 14 Neuromuscular Disease




Guillain Barre Syndrome American Academy Of Pediatrics
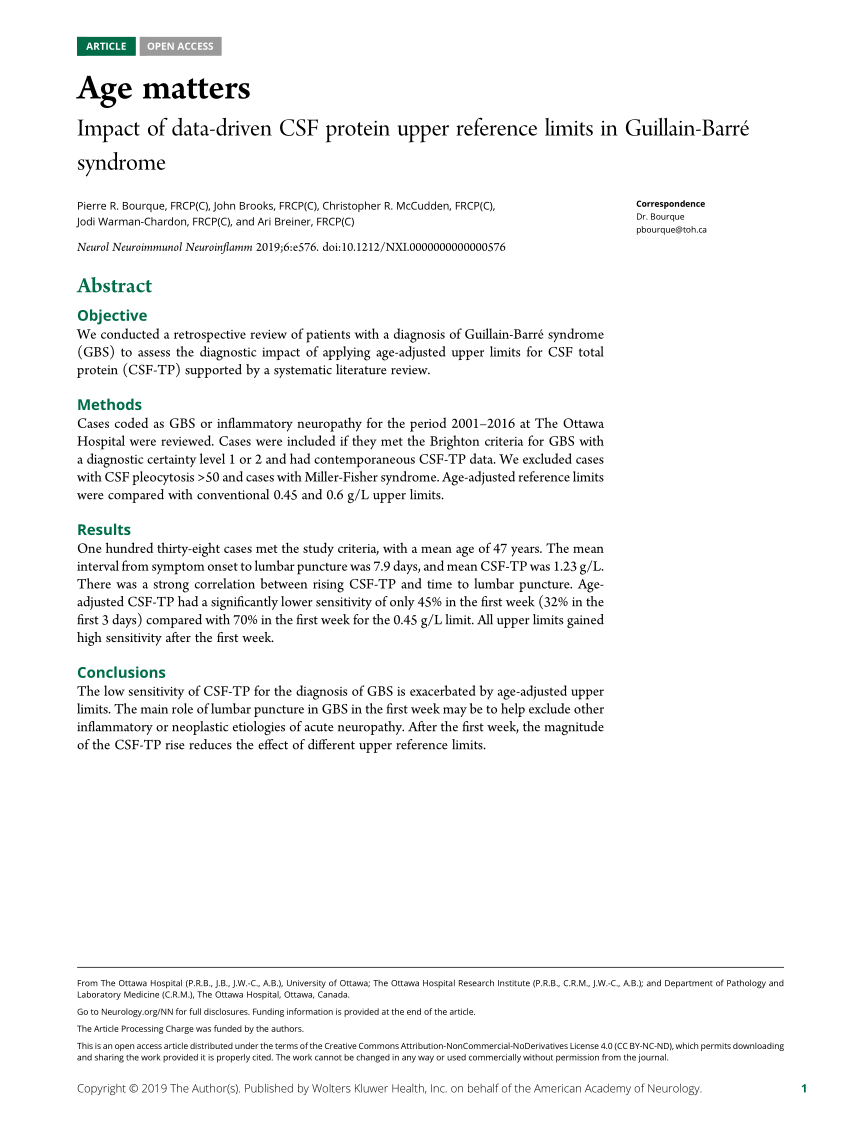



Pdf Age Matters Impact Of Data Driven Csf Protein Upper Reference Limits In Guillain Barre Syndrome



Pdf Guillain Barre Syndrome Semantic Scholar




Cerebrospinal Fluid Protein In Guillain Barre Syndrome Need For Age Dependent Interpretation Hegen 21 European Journal Of Neurology Wiley Online Library




The Guillain Barre Syndrome Nejm




The Guillain Barre Syndrome Report Of A Case Treated With Acth And Cortisone Nejm




Proteome Analysis Of Cerebrospinal Fluid In Guillain Barre Syndrome Gbs Journal Of Neuroimmunology




Scielo Brasil Guillain Barre Syndrome In The Elderly Clinical Electrophysiological Therapeutic And Outcome Features Guillain Barre Syndrome In The Elderly Clinical Electrophysiological Therapeutic And Outcome Features




Laboratory Findings At Initial Presentation And Recurrence Of Download Table



1
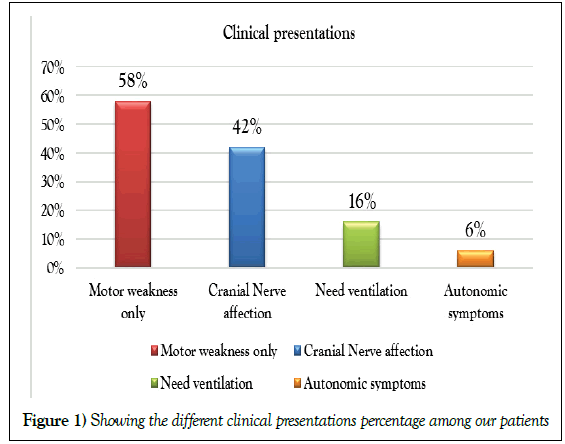



Factors Associated With Prognosis Of Guillain Barre Syndrome




Covid 19 And Guillain Barre Syndrome A Wellcome Open Research



2




Guillain Barre Syndrome Associated With Sars Cov 2 Nejm




Clinical Significance Of Serum And Csf Findings In The Guillain Barre Syndrome And Related Disorders Semantic Scholar




Guillain Barre Syndrome Associated With Jev Infection Nejm
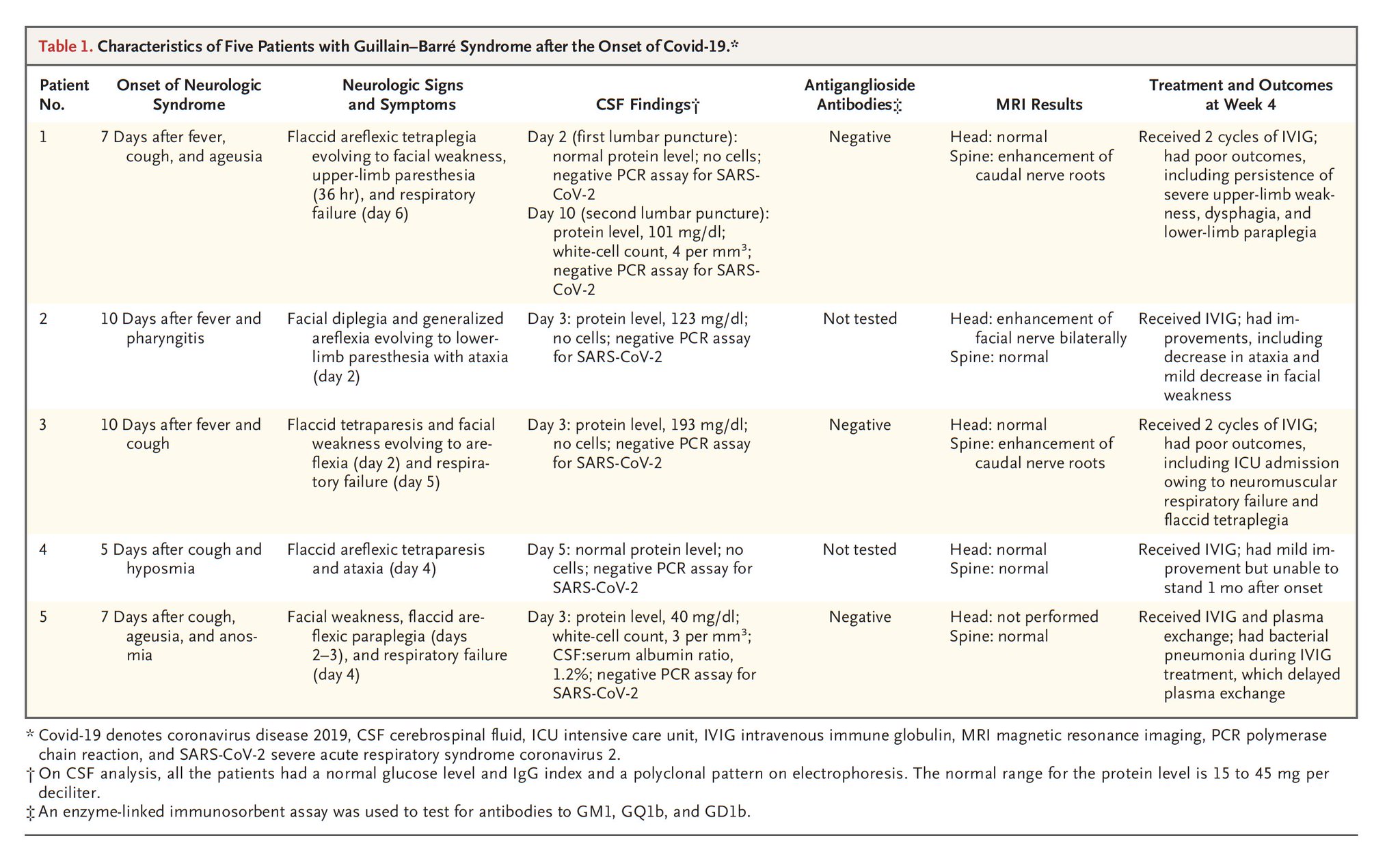



Eric Topol A Guillain Barre Syndrome In 5 Patients Who Were Infected W Covid19 T Co Zkjtake9x9 This Report From Centers From Italy Adds To The Other Central Nervous System Involvement T Co Bmppll3ava
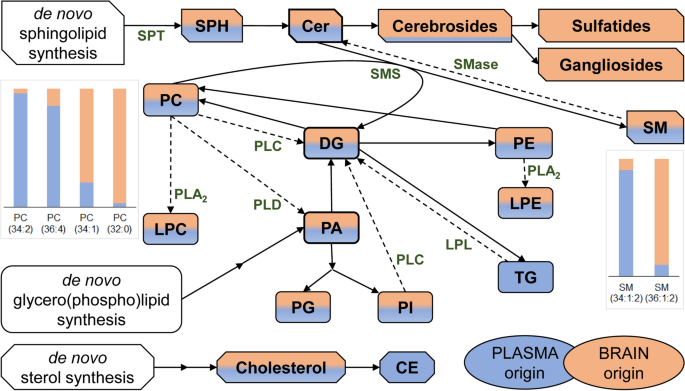



Cerebrospinal Fluid Lipidomic Biomarker Signatures Of Demyelination For Multiple Sclerosis And Guillain Barre Syndrome Scientific Reports




Increased Cerebrospinal Fluid Protein And Motor Conduction Studies As Prognostic Markers Of Outcome And Nerve Ultrasound Changes In Guillain Barre Syndrome Journal Of The Neurological Sciences



1




Guillain Barre Syndrome




Pdf Are Cerebrospinal Fluid Protein Levels And Plasma Neutrophil Lymphocyte Ratio Associated With Prognosis Of Guillain Barre Syndrome Semantic Scholar




Lightning Learning Guillain Barre Syndrome Em3 East Midlands Emergency Medicine Educational Media
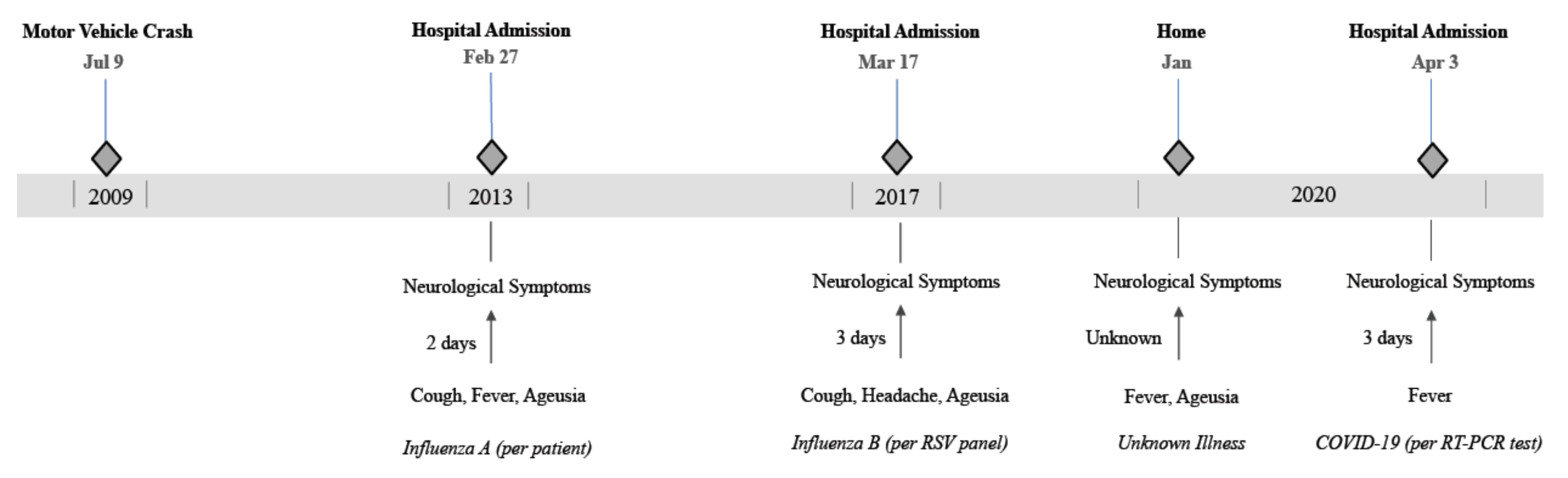



Pathogens Free Full Text Covid 19 As A Trigger Of Recurrent Guillain Barre Syndrome Html



Guillain Barre Syndrome Ppt Download




Guillain Barre Syndrome




Clinical Features And Csf Protein Levels In 12 Patients With Recurrent Gbs Download Table




Guillain Barre Syndrome Outbreak Associated With Zika Virus Infection In French Polynesia A Case Control Study The Lancet




Review Article On Covid 19 And Guillain Barre Syndrome




Pdf An Unusual Case Of Recurrent Guillain Barre Syndrome With Normal Cerebrospinal Fluid Protein Levels A Case Report



Headache And Papilledema In Guillain Barre Syndrome Canadian Journal Of Neurological Sciences Cambridge Core




Guillain Barre Syndrome American Family Physician



Manifestaciones Neurologicas De La Infeccion Por El Virus Zika



Guillain Barre Syndrome A Century Of Progress Nature Reviews Neurology




Age Matters Neurology Neuroimmunology Neuroinflammation




Biomarkers Of Guillain Barre Syndrome Some Recent Progress More Still To Be Explored




Clinical Significance Of Serum And Csf Findings In The Guillain Barre Syndrome And Related Disorders Semantic Scholar



Cerebrospinal Fluid Total Protein In Guillain Barre Syndrome Variants Correlations With Clinical Category Severity And Electrophysiology Springerlink



Www Gbs Cidp Org Wp Content Uploads 14 01 14 Fokke Gbs Brighton Brain 14 Pdf




Xmlinkhub



Guillain Barre Syndrome Rcemlearning




Increased Intracranial Pressure Caused By Increased Protein Content In The Cerebrospinal Fluid An Explanation Of Papilledema In Certain Cases Of Small Intracranial And Intraspinal Tumors And In The Guillain Barre Syndrome



Guillain Barre Syndrome




A Comprehensive Systematic Review Of Csf Analysis That Defines Neurological Manifestations Of Covid 19 International Journal Of Infectious Diseases




Clinical Variants Of Guillain Barre Syndrome In Children Pediatric Neurology




Guillain Barre Syndrome



Www Orpha Net Data Patho Pro En Guillainbarre Frenpro4v01 Pdf




Guillain Barre Syndrome The Lancet



Guillain Barre Syndrome Pathogenesis Diagnosis Treatment And Prognosis Nature Reviews Neurology



Guillain Barre Syndrome Gbs Emcrit Project




Guillain Barre Syndrome Nejm




Causes Of Albuminocytological Dissociation And The Impact Of Age Adjusted Cerebrospinal Fluid Protein Reference Intervals A Retrospective Chart Review Of 2627 Samples Collected At Tertiary Care Centre Bmj Open
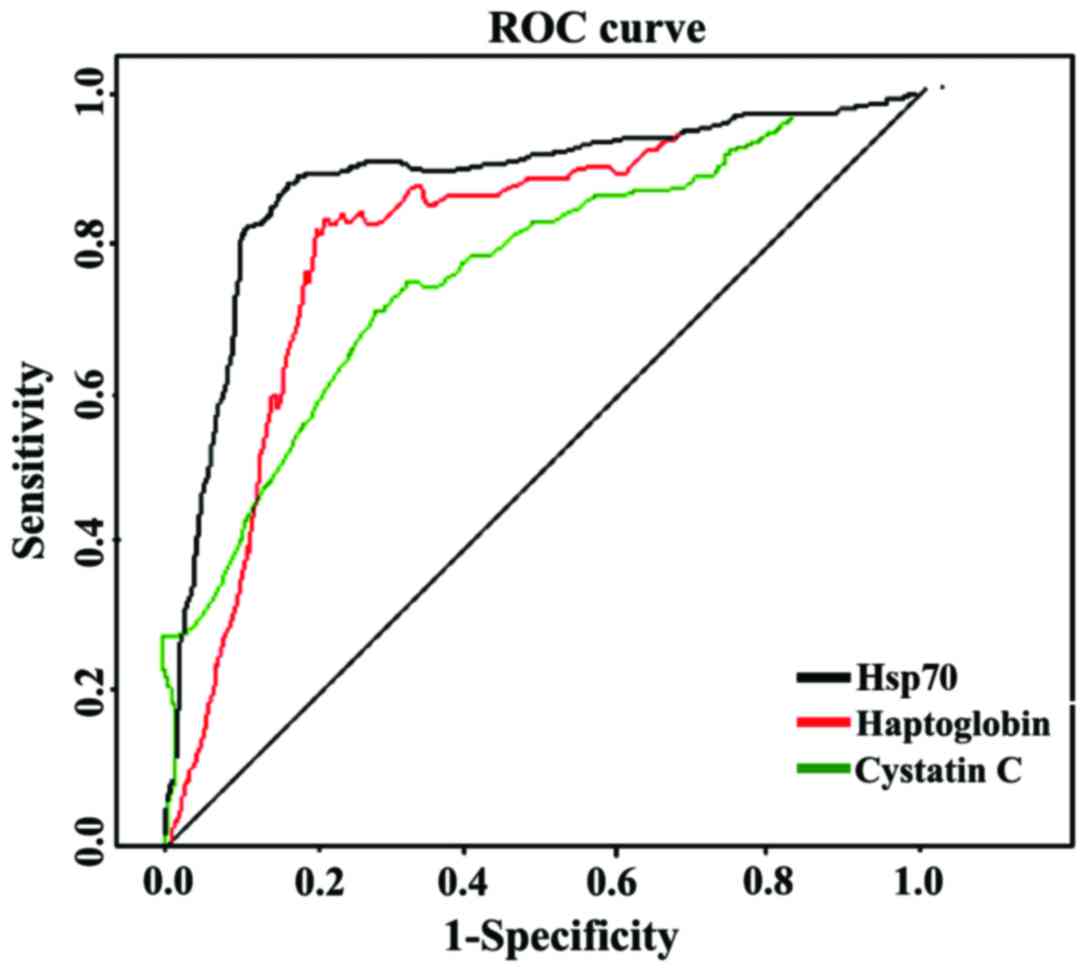



Identification Of Csf Biomarkers By Proteomicsin Guillain Barre Syndrome




Causes Of Albuminocytological Dissociation And The Impact Of Age Adjusted Cerebrospinal Fluid Protein Reference Intervals A Retrospective Chart Review Of 2627 Samples Collected At Tertiary Care Centre Bmj Open
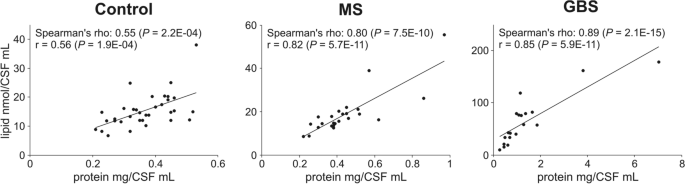



Cerebrospinal Fluid Lipidomic Biomarker Signatures Of Demyelination For Multiple Sclerosis And Guillain Barre Syndrome Scientific Reports
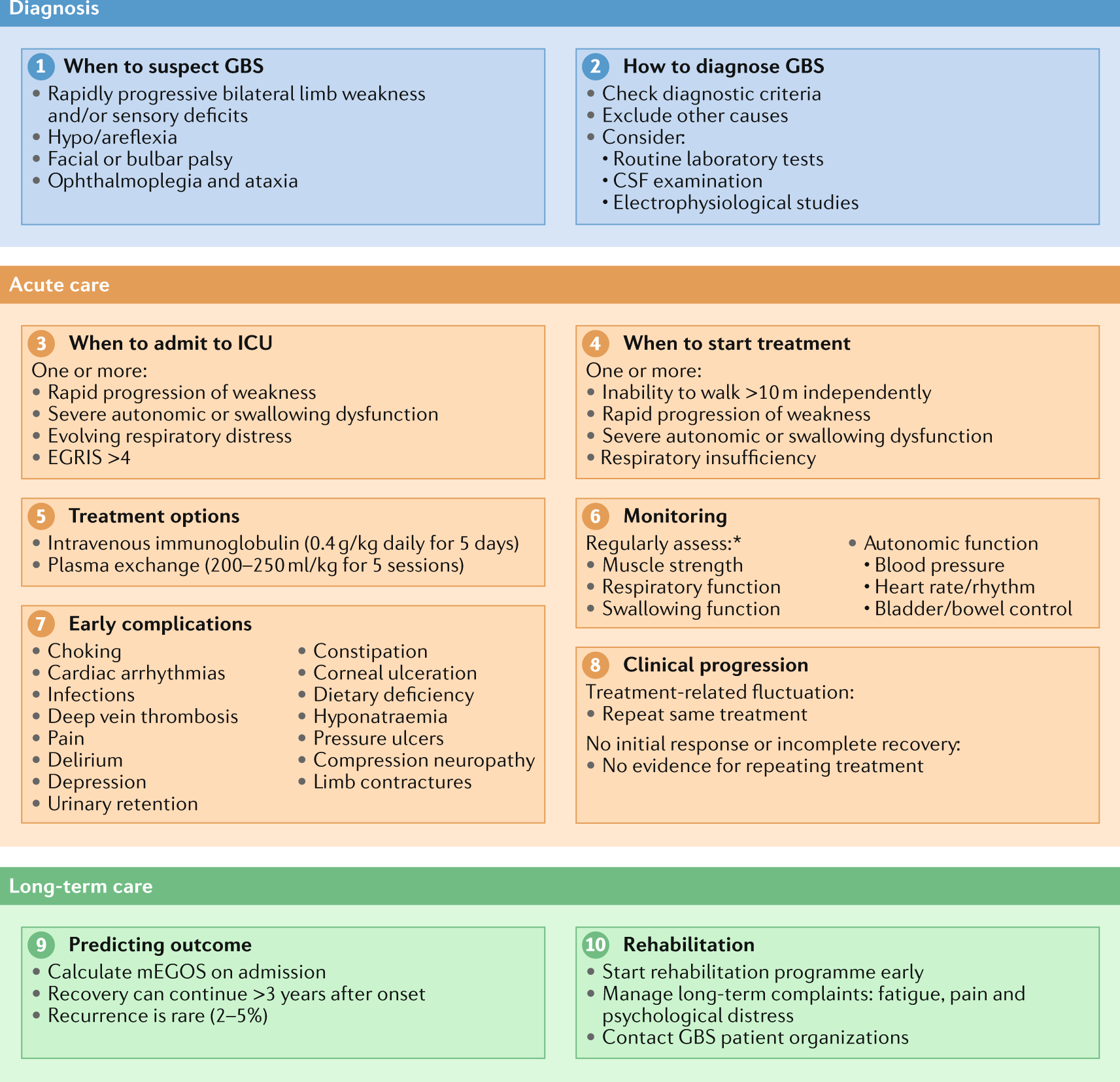



Diagnosis And Management Of Guillain Barre Syndrome In Ten Steps Nature Reviews Neurology



Guillain Barre Syndrome Immunology Microbiology Flashcards Draw It To Know It
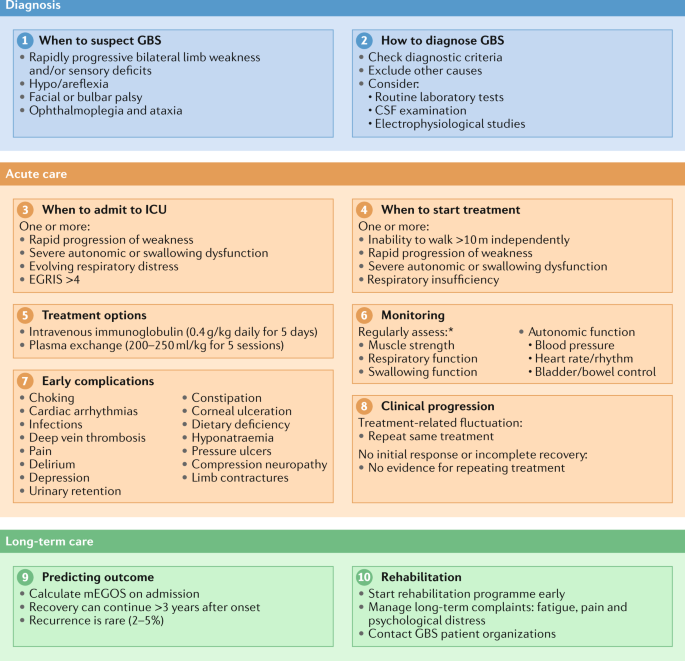



Diagnosis And Management Of Guillain Barre Syndrome In Ten Steps Nature Reviews Neurology



Cerebrospinal Fluid Analysis In Guillain Barre Syndrome Value Of Albumin Quotients Springerlink




Guillain Barre Syndrome American Family Physician



Improved A Guillain Barre Syndrome Patient With Positive Pcr Test For Coronavirus In Cerebrospinal Fluid After Plasmapheresis A Case Report Jentashapir Journal Of Cellular And Molecular Biology Full Text



Cerebrospinal Fluid Total Protein In Guillain Barre Syndrome Variants Correlations With Clinical Category Severity And Electrophysiology Request Pdf




Pdf Diagnosis Of Guillain Barre Syndrome And Validation Of Brighton Criteria Semantic Scholar



Cerebrospinal Fluid Analysis Part 2 Csf Complete Examination Normal Abnormal Labpedia Net



Emdocs Net Emergency Medicine Educationguillain Barre Syndrome Third Time S The Charm Emdocs Net Emergency Medicine Education



Pdf An Unusual Case Of Recurrent Guillain Barre Syndrome With Normal Cerebrospinal Fluid Protein Levels A Case Report




Guillain Barre Syndrome Knowledge Amboss




Pdf Guillain Barre Syndrome A Century Of Progress Semantic Scholar



Csf




Cerebrospinal Fluid Protein In Guillain Barre Syndrome Need For Age Dependent Interpretation Hegen 21 European Journal Of Neurology Wiley Online Library




Frontiers Immune Cell Profiling Of The Cerebrospinal Fluid Provides Pathogenetic Insights Into Inflammatory Neuropathies Immunology
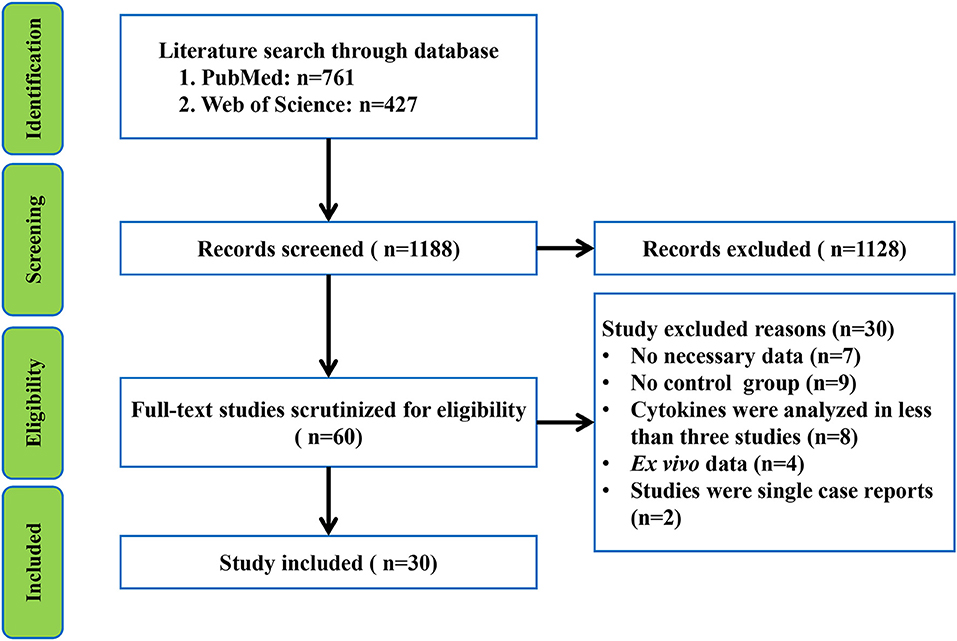



Frontiers Peripheral Blood And Cerebrospinal Fluid Cytokine Levels In Guillain Barre Syndrome A Systematic Review And Meta Analysis Neuroscience




Guillain Barre Syndrome The Lancet



Cerebrospinal Fluid Interpretation Csf Interpretation Geeky Medics


